Clinical Services
Division of Pain Medicine
Introduction
The Division of Pain Medicine in Department of Anaesthesiology, Queen Mary Hospital (QMH DA) is responsible for taking care of patients who are suffering from acute, chronic and cancer pain problems. Pain are referred from other medical specialists and health care professionals and seen at inpatient or outpatient clinics.
Structure
Director of Division (HKU and QMH)Prof. Chi Wai CHEUNG
MBBS, MD, FHKCA, FFPMANZCA, FHKAM(Anaesthesiology), Dip Pain Mgt (HKCA)
Clinical Professor, Department of Anaesthesiology, The University of Hong Kong
Director, Laboratory and Clinical Research Institute for Pain, The University of Hong Kong
Honorary Consultant, Queen Mary Hospital, Grantham Hospital, Duchess of Ken Children Hospital
Clinical Director & Supervisor of Training (Pain Fellowship)
Dr. Timmy Chi Wing CHAN
MBBS, FIPP, FANZCA, FHKCA, FHKAM(Anaesthesiology), FFPMANZCA, FHKCA(Pain Medicine), Dip of Pain Mgt (HKCA)
Consultant Anaesthetist
Honorary Clinical Associate Professor, Department of Anaesthesiology, The University of Hong Kong
Acute Pain Coordinator
Dr. Stanley Sau Ching WONG
MBBS, MD, FHKCA, FHKAM(Anaesthesiology), FANZCA, FHKCA(Pain Med)
Clinical Associate Professor, Department of Anaesthesiology, The University of Hong Kong
Honorary Associate Consultant(Anaesthesiology), Queen Mary Hospital
Chronic Pain Coordinators
Dr. Carrie Fung Ping WONG
MBBS, MMedSc, MRCP (UK), FANZCA, FHKCA, FHKCP, FHKAM (Anaesthesiology), FHKAM (Medicine)
Consultant Anaesthetist
Honorary Clinical Assistant Professor, Department of Anaesthesiology, The University of Hong Kong
Dr. Yiu Chung LAU
MBCHB, FHKCA, FHKAM(Anaesthesiology, FHKCA(Pain Med)
Associate Consultant Anaesthetist
Honorary Clinical Assistant Professor, Department of Anaesthesiology, The University of Hong Kong
Nursing Team
Ms. Shirley Wing Yi NG
Advanced Practice Nurse
MNurs, BN
RN, Post Registration Certificate Course in Perioperative Nursing, Post Registration Certificate Course in Pain Management
Ms. Wai Yi KONG
Advanced Practice Nurse
BHCSc(Nur), MHCM
RN, FHK College of Perioperative Nursing
Ms. Wing Yi PUN
Registered Nurse
BN
RN
Ms. Christy Ho Kei CHAN
Registered Nurse
BN, Higher Diploma in General Nursing
RN, Post Registration Certificate Course in Palliative Care
Ms. Hiu Yi LEE
Registered Nurse
MNurs, BN
RN
History
The QMH DA has been providing regular pain management services in QMH since 1990. This is the first formal pain management service in Hong Kong. The scope of services includes acute pain service (APS)—providing postoperative and other acute pain management; as well as chronic or cancer pain management—attending to all in-patient consultations from other specialties (with subsequent follow up care). The first out-patient clinic in pain management was jointly established by Department of Clinical Oncology and Department of Anaesthesiology in 1993. It serves patients with intractable cancer pain. The Division's own Pain Clinic was commenced in 1995 to look after out-patient referrals. In 1997, QMH DA was accredited by the Hong Kong College of Anaesthesiologists and became one of the first training centers of Diploma in Pain Management.
Scope of Clinical Services
Currently, the DA Division of Pain Medicine provides a comprehensive scope of pain management services in the QMH. These include APS, Chronic and Cancer pain management services (CPS).APS
Our APS focuses on pain management of patients after major operations (more than 3,200 patients were treated in 2010 alone). We also receive other pain consultations to manage patients suffering from thermal injury and traumatic painful conditions (e.g. rib fractures). Analgesic medications, patient-controlled analgesia (PCA), epidural analgesia and nerve/plexus blocks are commonly used. The patients are reviewed daily by anesthesiologists and a pain nurse. A twenty-four hour acute pain service is provided by the Department's Emergency Team. On top of this, a member of the Division of Pain Medicine is designated to provide tertiary consultation on 24 hour basis upon the Emergency Team's request.
The Division offers various protocols for acute pain management and patient monitoring. Because of these, high quality acute pain service could be carried out in different clinical areas e.g. the intensive care unit, high dependency unit and general wards. To ensure quality of care, implementation of APS protocols and patient monitoring are supervised by the Pain Nurse, who conducts a daily ward round with anaesthesiologists, as well as providing regular training to ward nurses.
Chronic Pain Service
Our CPS provides a comprehensive tertiary pain management service to both in-patients and out-patients, who are suffering from cancer pain or chronic (non-cancer) pain. We provide regular out-patient Pain Clinic Sessions, as well as Joint Outpatient Pain Clinic Sessions with the Department of Clinical Oncology (for cancer pain patients). CPS commences as soon as we received referrals from other medical specialties. After thorough patient assessment, we will formulate a pain management plan/schedule which is tailor-made to the patient. Treatment modalities ranging from simple analgesic regimens to more sophisticated therapies are provided. These include interventional pain procedures, cognitive behavioral therapy (the SMILE Program) and other multidisciplinary pain management involving other health care teams.
Multidisciplinary involvement is almost mandatory in modern pain medicine. The Division works in close collaboration with other medical specialists, clinical psychologists, physiotherapists, occupational therapists as well as medical social workers in the Hong Kong West Cluster. We play a coordinating role in this multidisciplinary team so as to provide holistic care to our patients. This is achieved through effective patient referral system as well as interdisciplinary case conferences.
Medical Records and Quality Assurance
All APS and CPS patients, have special medical records, both in hardcopies and electronic copies to ensure accurate documentation of diagnosis, treatment and progress. These records are managed by a designated clerical officer of the Division and strict protocols are in place to ensure patient confidentiality. Medical reports are issued upon request by the patient or other medical teams through proper hospital request channels. Moreover, patient care data are computerized for analysis to allow clinical audit and quality assurance activities.
Training Activities
The Division of Pain Medicine is committed to the training of pain specialists, anaesthetic vocational trainees, pain nurses and medical students. The Hong Kong College of Anaesthesiologists has accredited two training posts for the Diploma in Pain Management since 1997. 26 pain physicians have graduated so far. All of them excel at pain medicine, delivering specialist care to acute, chronic and cancer pain patients. The Division also welcomes overseas clinicians for training in pain medicine. Short term clinical attachment and fellowship appointments up to one year are provided.
Academic Activities
In addition to clinical services, the Division of Pain Medicine also conducts research, in collaboration with the Department of Anaesthesiology, The University of Hong Kong. Numerous original articles, published in international peer-reviewed journals, and two medical textbooks and MD Thesis in pain medicine were harvested from this fertile ground of clinical research.
Academic Output, Division of Pain Medicine, DA QMH
Medical Textbooks- A Guide to Pain Medicine, edited by Joseph C.S. Yang and S.L. Tsui, Hong Kong University Press May 2002. ISBN 962 209 544 5.
- Pain Medicine, a Multidisciplinary Approach, edited by S.L. Tsui, P.P Chen and Jacobus K.F. Ng, Hong Kong University Press August 2010. ISBN 978-988-8028-16-0.
MD Thesis, The University of Hong Kong
- Tsui SL. Postoperative Analgesia in Chinese Patients: An In-depth Analysis of Postoperative Pain Management in the Queen Mary Hospital of Hong Kong (1997).
- Cheung CW. Role of Dexmedetomidine in Acute Postoperative Pain Management (2011).
Publications in Peer Reviewed Journals
- Yeung SC, Irwin MG, Cheung CW. Environmental Enrichment in Postoperative Pain and Surgical Care: Potential Synergism with the Enhanced Recovery After Surgery Pathway. Ann Surg 2021; 273(1): 86-95.
- Wong SS, Cheung CW. Optimization of opioid utility in cancer pain populations. Ann Palliat Med 2020; 9(2): 558-70.
- Wong SSC, Chan WS, Cheung CW. Analgesic Effects of Cannabinoids for Chronic Non-cancer Pain: a Systematic Review and Meta-Analysis with Meta-Regression. J Neuroimmune Pharmacol 2020; 15(4): 801-9 Review.
- Wong SSC, Cheung CW. Analgesic Efficacy and Adverse Effects of Meperidine in Managing Postoperative or Labor Pain: A Narrative Review of Randomized Controlled Trials. Pain Physician 2020; 23(2): 175-201.
- Cheung CW. Epidural steroids - are we following the guidelines? Anaesthesia 2019; 74(12): 1500-03.
- Wong SS, Sun L, Qiu Q, Gu P, Li Q, Wang XM, Cheung CW. Propofol attenuates postoperative hyperalgesia via regulating spinal GluN2B-p38MAPK/EPAC1 pathway in an animal model of postoperative pain. Eur J Pain 2019; 23(4): 812-22.
- Wong SCS, Leung MYY, Cheung CW. The effect of total intravenous anaesthesia with propofol on postoperative pain after third molar surgery: a double blind randomized controlled trial. Eur J Pain 2019; 23(5): 884-93.
- Wong SCS, Lee UM, Wang XMA, Chung SK, Cheung CW. Role of DLC2 and RhoA/ROCK pathway in formalin induced inflammatory pain in mice. Neurosci Lett 2019; 709: 134379.
- Sun L, Li H, Tai LW, Gu P, Cheung CW. Adiponectin regulates thermal nociception in a mouse model of neuropathic pain. Br J Anaesth 2018; 120(6): 1356-67.
- Pan Z, Shan Q, Gu P, Wang XM, Tai LW, Sun M, Luo X, Sun L, Cheung CW. miRNA-23a/CXCR4 regulates neuropathic pain via directly targeting TXNIP/NLRP3 inflammasome axis. J Neuroinflammation 2018; 15(1): 29.
- Tai LW, Pan Z, Sun L, Li H, Gu P, Wong SSC, Chung SK, Cheung CW. Suppression of Pax2 atenuates allodynia and hyperalgesia through ET-1-ETAR-NFAT5 signaling in a rat model of neuropathic pain. Neuroscience 2018; 384(5): 139-51.
- Gu P, Wang XM, Sun L, Tai LW, Pan Z, Cheung CW. Histon deacetylase 5 (HDAC5) regulates neuropathic pain through SRY-related HMG-box 10 (SOX10)-dependent mechanism in mice. Pain 2018; 159(3): 526-39.
- Wong SS, Choi SW, Cheung CW. A comparison of chronic pain with and without neuropathic characteristics in a Hong Kong Chinese population: an analysis of pain related outcomes and patient help seeking behaviour. PLoS One 2018; 13(10): e0204054.
- Choi SW, Lam DM, Wong SSC, Shiu HH, Wang AX, Cheung CW. Effects of single nucleotide polymorphisms on surgical and post-surgical opioid requirements - a systematic review and meta-analysis. Clin J Pain 2017; 33(12): 1117-30.
- Sun L, Tai L, Qiu Q, Mitchell R, Fleetwood-Walker S, Joosten EA, Cheung CW. Endocannabinoid activation of CB1 receptors contributes to long-lasting reversal of neuropathic pain by repetitive spinal cord stimulation. Eur J Pain 2017; 21(5): 804-14.
- Qiu Q, Sun L, Wang XM, Lo ACY, Wong KL, Gu P, Wong SCS, Cheung CW. Propofol produces preventive analgesia via GluN2B-containing NMDA receptor/ERK1/2 signaling pathway in a rat model of inflammatory pain. Molecular Pain 2017; 13: 1-13.
- Cheung CW, Wong SSC, Qiu Q and Wang X. Oral oxycodone for acute postoperative pain: a review of clinical trials. Pain Physician 2017; 20(2S): SE33-52.
- Cheung CW, Choi SW, Wong SSC, Lee Y, Irwin MG. Changes in prevalence, outcomes and help-seeking behavior of chronic pain in an aging population over the last decade. Pain Practice 2017; 17(5): 643-54.
- Qiu Q, Choi SW, Wong SSC, Irwin MG, Cheung CW. Effects of intra-operative maintenance of general anaesthesia with propofol and postoperative pain outcomes - a systematic review and meta-analysis. Anaesthesia 2016; 71(10): 1222-33.
- Cheung CW*, Chan TCW, Chen PP, Chu MC, Chui WCM, Ho PT, Lam F, Law SW, Lee JYL, Wong SHS, Wong VKC. Opioid therapy for chronic non-cancer pain: guidelines for Hong Kong. Hong Kong Med J 2016; 22(5): 496-505.
- Luo X, Tai WL, Sun L, Pan Z, Xia Z, Chung SK, Cheung CW. Crosstalk between astrocytic CXCL12 and microglial CXCR4 contributes to the development of neuropathic pain. Molecular Pain 2016 Mar; 12: 1744806916636385.
- Cheung CW. Prescription drug monitoring programs needed to manage opioid use in asia pacific. Pain Practice 2016; 16(5): E93.
- Chan AC, Qiu Q, Choi SW, Wong SS, Chan AC, Irwin MG, Cheung CW. Effects of intra-operative total intravenous anaesthesia with propofol versus inhalational anaesthesia with Sevoflurane on post-operative pain in liver surgery: a retrospective case-control study. PLoS One 2016; 11(2): e0149753.
- Hung VKL, Tai LW, Luo X, Wang XA, Chung SK, Cheung CW. Targeted overexpression of astrocytic endothelin-1 attenuates neuropathic pain by upregulating spinal excitatory amino acid transporter-2. J Mol Neurosci 2015; 57(1): 90-6.
- Cheung CW, Qiu Q, Ying AC, Choi SW, Law WL, Irwin MG. The effects of intraoperative dexmedetomidine on postoperative pain, side-effects and recovery in colorectal surgery. Anaesthesia 2014; 69(11): 1214-21.
- Hung KL, Tai W, Qiu Q, Luo X, Wong KL, Chung SK, Cheung CW. Over-expression of astrocytic ET-1 attenuates neuropathic pain by inhibition of ERK 1/2 and Akt(s) via activation of ETA receptor. Mol Cell Neurosci 2014; 60: 26-35.
- Cheung CW, Qiu Q, Choi SW, Moore B, Goucke R, Irwin MG. Chronic opioid therapy for chronic non-cancer pain: a review and comparison of treatment guidelines. Pain Physician 2014; 17: 401-14.
- Luo X, Tai WL, Sun LT, Qiu Q, Xia ZY, Chung SK, Cheung CW. Central administration of C-X-C chemokine receptor type 4 antagonist alleviates the development and maintenance of peripheral neuropathic pain in mice. PLOS One 2014; 9: e104860.
- Ng FY, Ng JKF, Chiu KY, Yan CH, Chan CW. Multimodal periarticular injection Vs continuous femoral nerve block after total knee arthroplasty: a prospective, crossover, randomized clinical trial. J Arthroplasty 2012 Jun; 27(6): 1234-8.
- Cheung CW, Choi WS, Leung YY, Lui F, Ng KFJ, Ho AMH, Irwin MG. A double blind randomized crossover study to evaluate the timing of pregabalin for third molar surgery under local anesthesia. J Oral Maxillofac Surg 2012 Jan; 70(1): 25-30.
- Hung KL, Chan MY, Tai W, Chen YS, Chung SK, Cheung CW. Over-expression of endothelin-1 in astrocytes, but not endothelial cells, ameliorates inflammatory pain response after formalin injection. Life Sci 2012; 91(13-14): 618-22.
- Cheung CW, Ng KFJ, Liu J, Yuen MYV, Ho MHA, Irwin MG. Analgesic and sedative effects of intranasal dexmedetomidine in third molar surgery under local anaesthesia. Br J Anaesth 2011 Sep; 107(3): 430-7.
- Cheung CW, Ng KFJ, Choi WS, Chiu WK, Ying CLA, Irwin MG. Evaluation of the analgesic efficacy of local dexmedetomidine application. Clin J Pain 2011 Jun; 27(5): 377-82.
- Chan BKB, Tam LK, Wat CY, Chung YF, Tsui SL, Cheung CW. Opioids in chronic non-cancer pain. Expert Opin Pharmacother 2011 Apr; 12(5): 705-20.
- Chan AKM, Cheung CW, Chong YK. Alpha-2 Agonists in Acute Pain Management. Expert Opin Pharmacother 2010; 11(17): 2849-68.
- Kong VKF, Irwin MG. Adjuvant analgesics in neuropathic pain. Eur J Anaesth 2009 Feb; 26(2): 96-100.
- Cheung CW, Ying CLA, Lee LHY, Tsang SF, Tsui SL, Irwin MG. An audit of postoperative intravenous patient-controlled analgesia with morphine: Evolution over the last decade. Eur J Pain 2009; 13(5): 464-71.
- Lee LH, Irwin MG, Yao TJ, Yuen MK, Cheung CW. Timing of intraoperative parecoxib analgesia in colorectal surgery. Acute Pain 2008; 10(3-4): 123-30.
- Cheung CW, Ying CLA, Chiu WK, Wong GTC, Irwin MG. A comparsion of dexmedetomidine and midazolam for sedation in third molar surgery. Anaesthesia 2007 Nov; 62(11): 1132-8.
- Kong VKF, Irwin MG. Gabapentin: a multimodal perioperative drug? Br J Anaesth 2007 Dec; 99(6): 775-86.
- Wong GT, Yuen VM, Chow BF, Irwin MG. Persistent pain in patients following scoliosis surgery. Eur Spine J 2007 Oct; 16(10): 1551-6.
- Ng KF, Yuen TS, Ng VM. A comparison of postoperative cognitive function and pain relief with fentanyl or tramadol patient-controlled analgesia. J Clin Anesth 2006 May;18(3): 205-10.
- Tsui SL, Yong BH, Ng KFJ, Yuen TST, Li CFC, Chui KY. Delayed epidural catheter removal: the impact of postoperative coagulopathy. Anaesth Intensive Care 2004; 32(5): 630-6.
- Mak PH, Irwin MG, Tsui SL. Functional improvement after physiotherapy with a continuous infusion of local anaesthetics in patients with complex regional pain syndrome. Acta Anaesthesiol Scand 2003 Jan; 47(1): 94-7.
- Yuen TS, Ng KF, Tsui SL. Neurolytic celiac plexus block for visceral abdominal malignancy: is prior diagnostic block warranted? Anaesth Intensive Care 2002; 30(4): 442-8.
- Mak PH, Tsui SL, Ng KF. Long-term therapy of chronic non-malignant pain with potent opioids in an active police officer. Can J Anaesth 2002 Jun; 49(6): 575-8.
- Ng KF, Tsui SL, Chan WS. Prevalence of common chronic pain in Hong Kong adults. Clin J Pain 2002 Sep-Oct;18(5): 275-81.
- Clark WC, Yang JCS, Tsui SL, Ng KF, Clark SB. Unidimensional pain rating scales: a multidimensional affect and pain survey (MAPS) analysis of what they really measure. Pain 2002 Aug; 98(3): 241-7.
- Leung CC, Chan YM, Ngai SW, Ng KF, Tsui SL. Effect of pre-incision skin infiltration on post-hysterectomy pain - a double-blind randomized controlled trial Anaesth Intensive Care 2000 Oct; 28(5): 510-6.
- Mak PH, Tsui SL, Ip WY, Irwin MG. Brachial plexus infusion of ropivacaine with patient-controlled supplementation. Can J Anaesth 2000 Sep; 47(9): 903-6.
- Yang JC, Clark WC, Tsui SL, Ng KF, Clark SB. Preoperative multidimensional affect and pain survey (MAPS) scores predict postcolectomy analgesia requirement. Clin J Pain 2000 Dec; 16(4): 314-20.
- Yong BH, Tsui SL, Leung CC, Lo CM, Liu CL, Fan ST, Young K. Management of postoperative analgesia in living liver donors. Transplant Proc 2000 Nov; 32(7): 2110.
- Tsui SL, Ng KFJ, Wong LC, Tang GWK, Pun TC, Yang JCS. Prevention of postoperative nausea and vomiting in gynaecological laparotomies: a comparison of tropisetron and ondansetron. Anaesth Intensive Care 1999 Oct; 27(5): 471-6.
- Ng KF, Tsui SL, Yang CS. Unilateral approach to posterior retrocrural coeliac plexus block. Chin Med J (Engl) 1999 Jan; 112(1): 89-92.
- Ng KFJ, Tsui SL, Yang JCS, Ho ETF. Increased nausea and dizziness when using tramadol for post-operative patient-controlled analgesia (PCA) compared with morphine after intraoperative loading with morphine. Eur J Anaesthesiol 1998 Sep; 15(5): 565-70.
- Tsui SL, Law S, Fok M, Lo JR, Ho E, Yang JCS, Wong J. Postoperative analgesia reduces mortality and morbidity after esophagectomy. Am J Surg 1997 Jun; 173(6): 472-8.
- Tsui SL, Irwin MG, Wong MLC, Fung KYS, Hui WCT, Ng KF, Chan WS, O'Regan AM. An audit of the safety of an acute pain service. Anaesthesia 1997 Nov; 52(11): 1042-7.
- Tsui SL, Lee DK, Ng KF, Chan TY, Chan WS, Lo JW. Epidural infusion of bupivacaine 0.0625% plus fentanyl 3.3 µg/ml provides better postoperative analgesia than patient-controlled analgesia with intravenous morphine after gynaecological laparotomy. Anaesth Intensive Care 1997 Oct; 25(5): 476-81.
- Chan WS, Peh W, Ng KF, Tsui SL, Yang JCS. Computed tomography scan-guided neurolytic superior hypogastric block complicated by somatic nerve damage in a severely kyphoscoliotic patient. Anesthesiology 1997 Jun; 86(6): 1429-30.
- Ng KF, Tsui SL, Yang JCS, Ho ETF. Comparison of tramadol and tramadol/droperidol mixture for patient controlled analgesia. Can J Anaesth 1997 Aug; 44(8): 810-5.
- Tsui SL, Tong WN, Irwin MG, Ng KFJ, Lo JR, Chan WS, Yang JCS. The efficacy, applicability and side-effect of postoperative intravenous patient-controlled morphine analgesia: an audit of 1233 Chinese patients. Anaesth Intensive Care 1996 Dec; 24(6): 658-64.
- Irwin MG, Campbell B, Tsui SL, Yang JCS. Patient maintained alfentanil target-controlled infusion for analgesia during extra-corporeal shock wave lithotripsy. Can J Anaesth 1996 Sep; 34(9): 919-24.
- Yang JCS, Ng KFJ, O'Regan AM, Tsui SL, Tong WN. Recent advances in opioid therapy. Hong Kong Med J 1996 Dec; 2(4): 397-400.
- Tsui SL, Ng KFJ, Chan WS, Chan TY, Lo JR, Yang JCS. Cancer pain management: experience of 702 consecutive cases in a teaching hospital in Hong Kong. Hong Kong Med J 1996 Dec; 2(4): 405-13.
- Tsui SL. Postoperative pain management: an update. The Cutting Edge 1995 (Dec).
- Tsui SL, Lo JR, Tong WN, Yang JCS, O'Regan AM, Ng KFJ, Lam CS. A Clinical Audit for Postoperative Pain Control on 1443 Surgical Patients. Acta Anaesthesiol Sin 1995 Sep; 33(3): 137-48.
- Tsui SL, Tong WN, Lam CS, Lo JR, O'Regan AM, Yang JCS. Cancer pain management: a recent experience by anaesthesiologists in a teaching hospital in Hong Kong. Acta Anaesthesiol Sin 1994 Sep; 32(3): 193-201.
- Tsui SL, Chan CS, Chan ASH, Wong SJ, Lam CS, Jones RDM. Postoperative analgesia for oesophagectomy: a comparison of three analgesic regimens. Anaesth Intensive Care 1991 Aug; 19(3): 329-37.

Postoperative Analgesia - Patient Controlled Analgesia (PCA) Machine

Postoperative Analgesia - Infusion Pump for Epidural Analgesia

Postoperative Pain Control - Thoracic Epidural Analgesia

Postoperative Pain Control - Supraclavicular Brachial Plexus Block Infusion

Sphenopalatine Ganglion Block (1)

Sphenopalatine Ganglion Block (2)

Percutaneous Radiofrequency Lesioning of Trigerminal Ganglion (1)

Percutaneous Radiofrequency Lesioning of Trigerminal Ganglion (2)
Percutaneous Radiofrequency Lesioning of Trigerminal Ganglion (3)

Cervical Facet Joint Injection

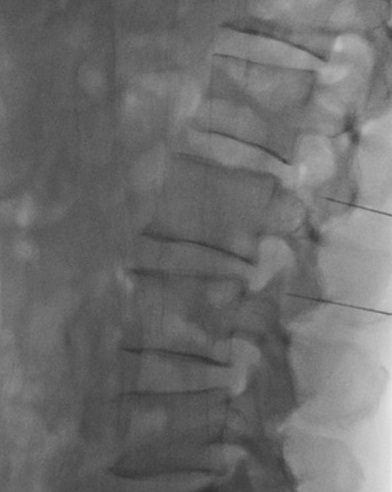
Lumbar Facet Joint Injection

Two Radiofrequency Lesioning Machines

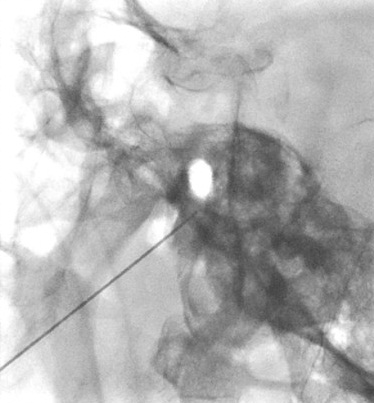
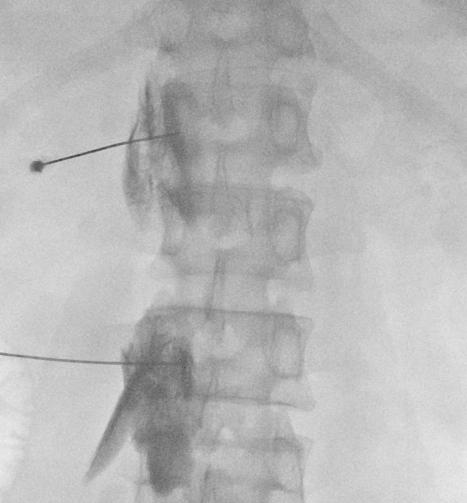
Percutaneous radiofrequency neurotomy of the lumbar medial branch nerves (1)

Percutaneous radiofrequency neurotomy of the lumbar medial branch nerves (2)
Percutaneous radiofrequency neurotomy of the lumbar medial branch nerves (3)
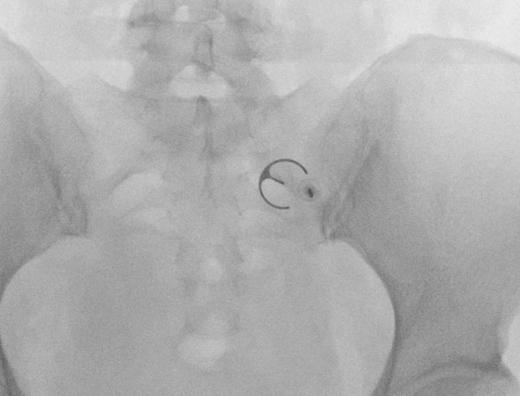
Cooled Radiofrequency for Sacroiliac Joint Pain

Lumbar Sympathetic Block - Neurolytic (1)
Lumbar Sympathetic Block - Neurolytic (2)

Caudal Epidural Steroid Injection (1)
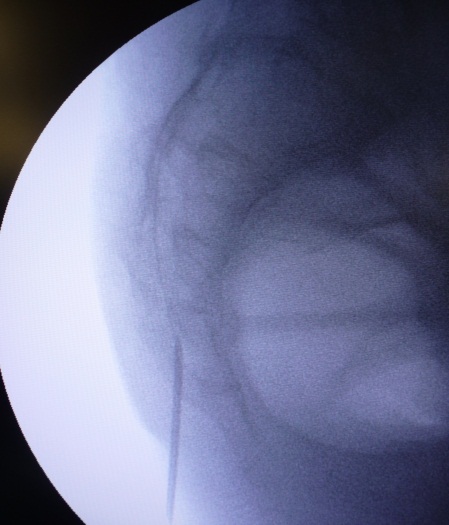
Caudal Epidural Steroid Injection (2)
Ganglion of Impar Block

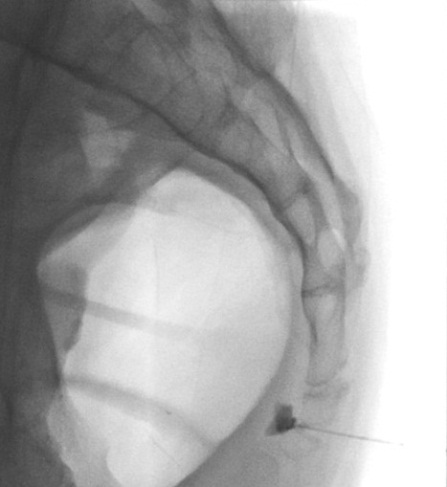
Coeliac Plexus Block (1)

Coeliac Plexus Block (2)

Coeliac Plexus Block (3)

Intercostal Nerve Block – Neurolytic
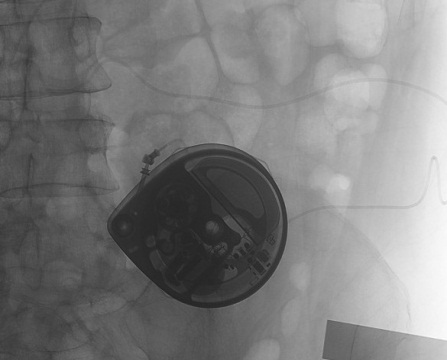
Intrathecal Pump Implantation
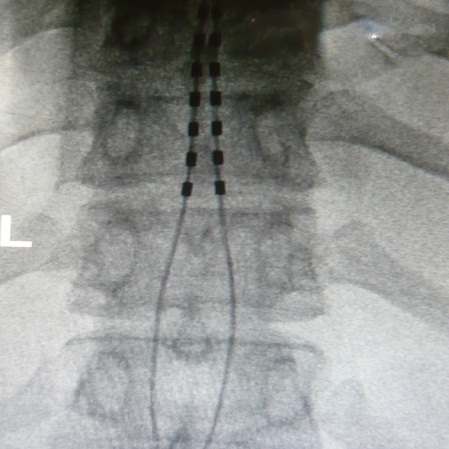
Spinal Cord Stimulator Implantation

Cognitive Behaviour Therapy - SMILE Program
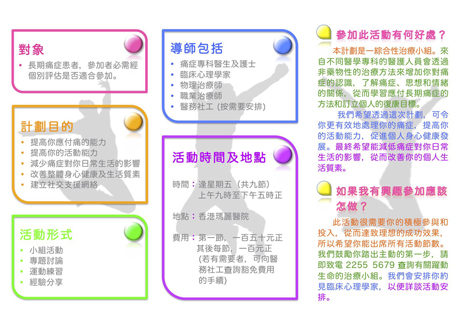
SMILE Program (1)
SMILE Program (2)

SMILE Program (3) – Relaxtion

SMILE Program (4) – Exercise

SMILE Program (5) – Sharing

